The minute health systems started shutting down services at the start of the COVID-19 pandemic, reality hit that something was broken.
It was more than the supply chain, which forced the rationing of personal protective equipment. It went beyond cleaning protocols as facilities tried to mitigate infection spread. It was greater than a need for more ICU beds and negative pressure rooms available to treat infected patients.
It was everything, from surge capacity to traffic flow, technology to staffing, The strain of closed clinics and operating rooms proved to be greater than many had anticipated, and coupled with overtime for other staff, and expenses for quick room conversions for negative air flow, the situation elicited one large question: “How did we get here?”
For more than a decade, the planning for healthcare organizations has been guided by the Institute for Healthcare Improvement’s Triple Aim – to improve the experience of care, population health, and the cost associated with care. That pursuit of the aim led to campuses and facilities that are more intuitive for patient-families, more efficient for staff, and more cost effective to operate…all in normal operations.
While an understatement, COVID-19 proved to be anything but normal, and in its sweep across the nation, it exposed a deficiency in our collective healthcare system. Missing from the Triple Aim was “resiliency,” a word often applied to physical structures, not so much to operations. As organizations pursued the Triple Aim, with a strategic and structural shift from inpatient to outpatient care, facilities and campuses reflected that shift, designed for consumers of care with a focus to keep the community healthy and reduce the need for hospitalization.
The flood of need for hospitalization in the pandemic isn’t an indictment that the previous pursuits were wrong. Rather, in exposing the gaps in healthcare operations, the pandemic has revealed the need to evolve our planning approaches. More than answering how organizations got here, the question is, “How do we move from here?”
A New Planning Approach
The scenario laid out by the pandemic is that: a scenario. On its own, COVID-19 represents a national event whose scale and impact has little precedent. However, in the past 15 years, the coronavirus spread is one of many unplanned events that have challenged both large and small organizations, alike. MERS, SARS, mass shootings, 100-year floods, tornadoes – the scenarios that strain the resources of hospitals, clinics, and the communities that they serve occur at a greater frequency that ever before.
Through that lens, we can both critique the plans that put organizations where they are now and evolve the process to find a resilient path to managing through these scenarios. Simply called Scenario Planning, this new approach to the traditional master planning process aims to mitigate the impacts scenarios can have on operations and facilities.
Most campuses and facilities have been programmed through a master planning process, a practice that usually relies on observed trends to forecast a probable future. What the current pandemic has shown is that the scenario under which the plans are crafted focus on a desirable future, one predicated that the future will be similar to the past. The master planning process often assumes an environment that operates business as usual, and the facilities and infrastructure are designed accordingly.
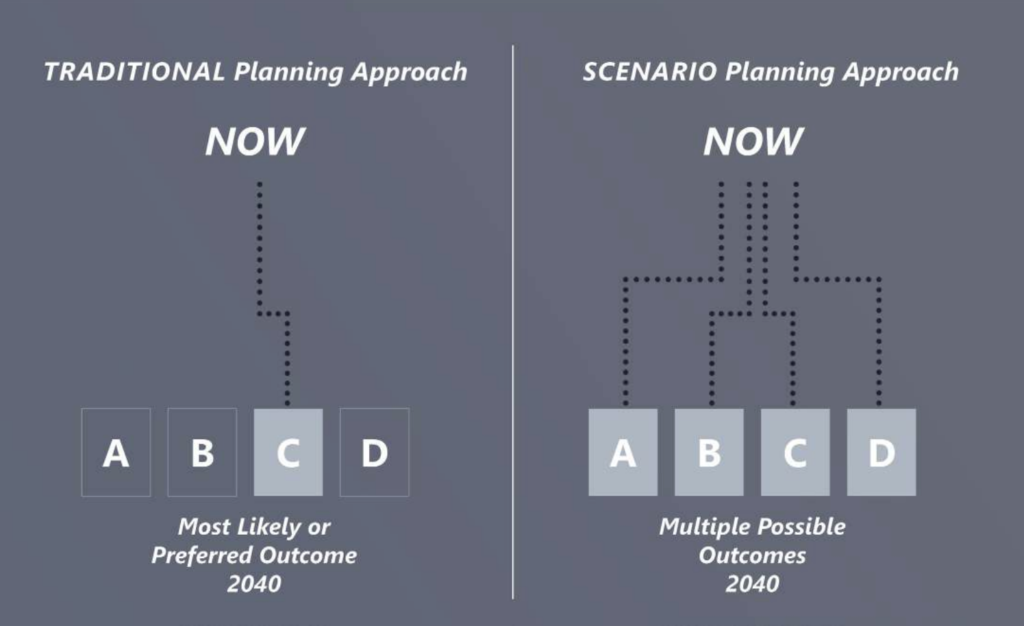
Scenario planning takes the planning process to a new level. More than planning for a worst-case scenario, scenario planning puts the integrity of an organization’s operations at the center of the planning process. A dynamic approach to planning, the planning process enables organizations to understand the possible effects unplanned, adverse events could have on their personnel, supplies, and facilities.
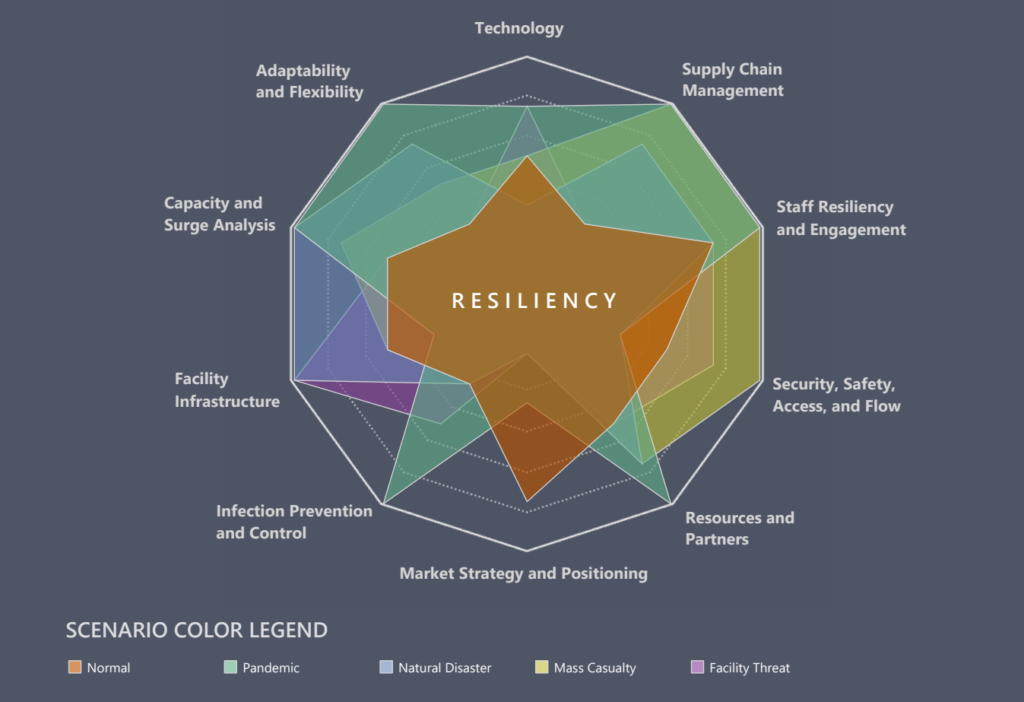
Where vision drives much of the master planning process, scenario planning complements that vision through a segmented analysis of the drivers of an organization’s operations. By studying the impacts scenarios have on each part of an organization’s operations, the organization is forced to consider enterprise-wide how it can respond to adverse conditions demanding rapid attention and adaptation. Beyond the response, the analysis concentrates the planning on how organizations can pivot facilities, technology, and personnel in a moment while protecting its ability to operate at optimum levels.
Resiliency Redefined
Scenario planning combines the vision of where organizations want to go under controlled conditions with an approach that examines that resiliency of the vision in the face of uncontrolled conditions. It takes the idea of resiliency in operations to expand its definition beyond recoverability. Instead of analyzing how quickly a normal state of operations can return after those operations are disrupted, scenario planning allows teams to consider how well the organization can absorb a disruption to maintain continuous operations.
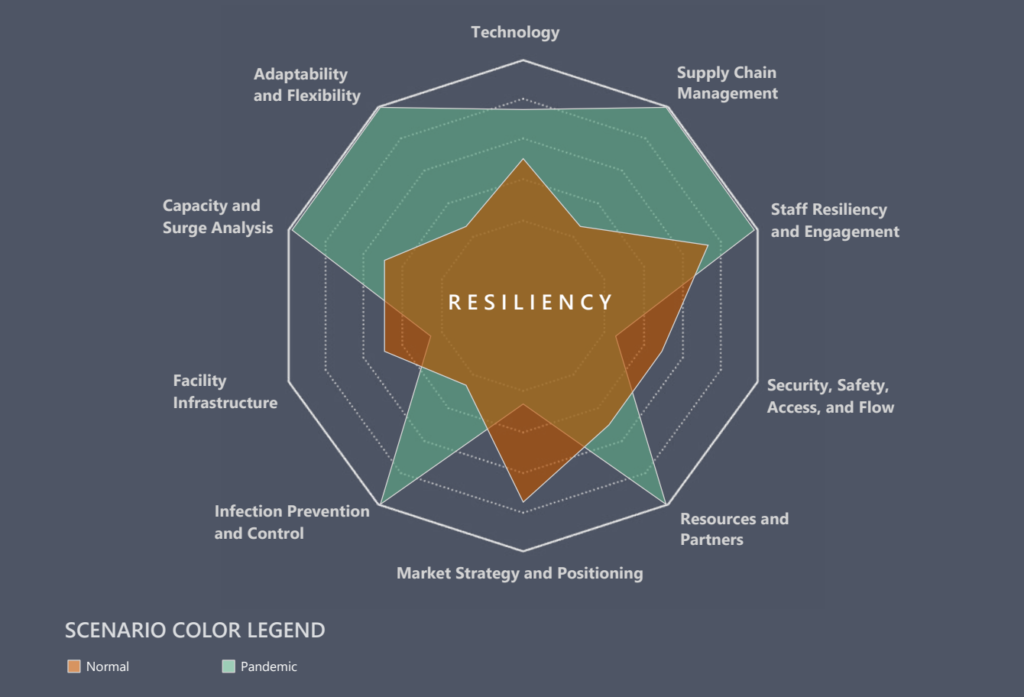
Facilities and infrastructure are then designed for disruption absorption – alternative care sites, alternative care delivery methods, flexible mechanical systems, adaptable spaces, alternative traffic flows, as well as support for staff wellness under unrelenting stress. By creating a dialogue between all the various parts of an organization, a dynamic plan is shaped to help organizations maintain the integrity of their operations through adversity.
According to a report from the American Hospital Association, shuttered and modified operations in response to COVID-19 has resulted in a 19.5% drop in inpatient volumes at non-federal hospitals, and an additional 34.5% drop in outpatient volumes. Losses from the first four months of the pandemic plus projected continued losses, even after services come back online, are expected to exceed $323 billion in 2020. (Click to read the report.)
The current pandemic represents a real existential threat for many healthcare organizations. The look of hospitals, clinics, and their operations after the pandemic will be different from what it was before the pandemic. However, “different” must be “better.” While COVID-19 provides a better understanding of how a pandemic can impact operations, it is only one of many scenarios that force organizations to deviate their operations from normal. Disruptions to operations will continue. Only through a better planning process can we mitigate the impacts those disruptions can have on the integrity of the whole healthcare organization.
Mike Boldenow is a principal at BWBR who has spent much of his career working with healthcare organizations to develop facilities that enhance the services they provide in both small communities and large metropolitan regions. Mike can be reached at mboldenow@bwbr.com or 651.290.1996. Scott Holmes, RA, ACHA, LEED AP, is a retired principal and healthcare planner who has worked with organizations from large health systems to critical access hospitals to program spaces that increase efficiencies and improve the delivery of care.








